All about rosacea and acne rosacea
/Rosacea is a chronic skin condition that most notably causes flushing and redness on the face. Just like acne, it’s a highly misunderstood condition and it’s often misdiagnosed. True rosacea is actually very rare and in the decade or so that I have been practicing, I have probably had over a hundred people who thought they had rosacea because they were diagnosed or they self-diagnosed and only 3 of those people actually had rosacea. Symptoms of rosacea might flare up then calm down in cycles but rosacea flare ups tend to last weeks or months whereas acne flare ups tend to last years.
ROSACEA IS OFTEN MISDIAGNOSED FOR THESE CONDITIONS
Acne rosacea is often confused for a type of acne called inflamed acne
Irritation from using skincare products that are too strong, irritating, or not appropriate for your skin type
Irritation from using skincare products that are not nourishing or moisturizing enough
Redness from chronic picking or post-inflammatory hyperpigmentation (PIH) which are dark marks leftover from inflamed acne or picking
Redness from having a genetic tendency to flush easily that is common in people with fair skin
SYMPTOMS
There are four subtypes of rosacea that I list below but there are some common symptoms that can occur with all of the subtypes:
Redness and flushing on the face or body that looks like a sunburn
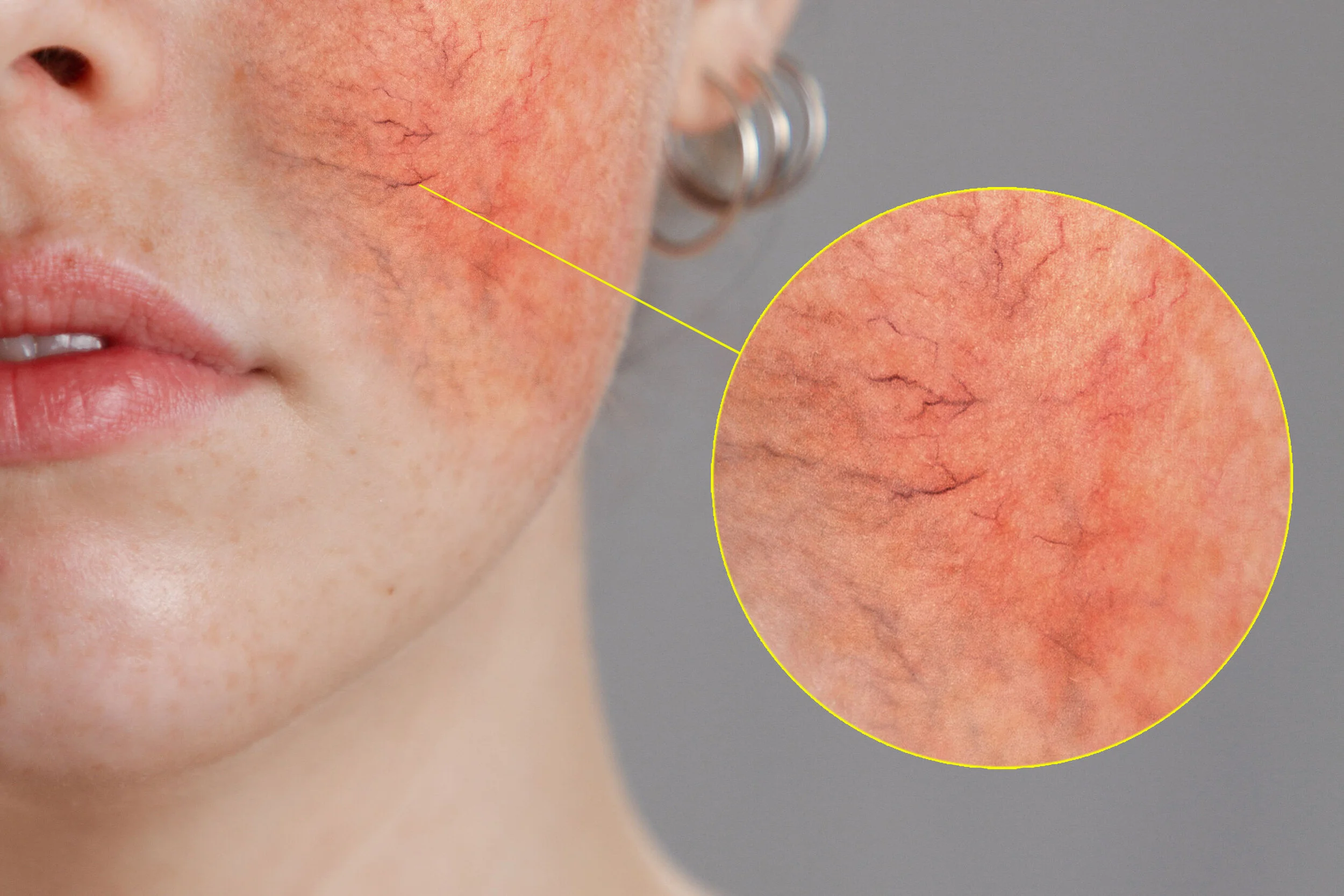
Broken blood vessels on your face or eyes that look like spider veins
Rough, raised, dry patches called plaques
Sensitivity, burning, stinging
Oils skin or enlarged pores
Bumpy skin texture
ROSACEA TYPES
You might have one or a combination of these subtypes and your type of rosacea might also shift throughout your life:
Subtype One: Erythematotelangiectatic Rosacea
This is the most well known form of rosacea characterized by persistent redness, flushing, and enlarged blood vessels.
Subtype Two: Papulopustular Rosacea
This is rosacea that occurs with acne-like breakouts. It can also show up as hardened patches called plaques and excessive oiliness.Subtype Three: Phymatous/Rhinophyma Rosacea
This is a rare type of rosacea that causes thickening skin on the cheeks, chin, forehead, ears, or nose (Rhinophyma).Subtype Four: Ocular Rosacea
This type of rosacea affects the eyes and can cause symptoms like pain, swelling, redness, and vision issues.
CAUSES
The cause of rosacea is unknown but, much like acne, it’s likely a multifactorial disease that is caused by the perfect storm of genes, internal factors, and external factors. There are theories that it might be caused by a bacteria called Helicobacter Pylori, an overgrowth of demodex mites, or a protein called cathelicidin that might cause redness and swelling. Similar to acne, there are many potential internal and external triggers that can initiate a flare up or exacerbate an existing flare up. Everyone has different triggers so you might be triggered by one or a combination of any of these:
Spicy foods
Hot drinks
Exercise
Cosmetics and skincare products
Certain drugs + medications
Extreme weather (cold or hot)
Sun exposure
Wind exposure
Stress
Heat, humidity
Alcohol
Smoking
Improper skincare routine (products that are too strong or not nourishing enough)
RISK FACTORS
Rosacea can affect anyone but these factors make it more likely:
Fair skinned people with blond hair, blue eyes, and European descent
Women are more like to develop rosacea than men
Rosacea usually affects people between the ages of 30-50
Family history of rosacea
Smoking can increase the risk
DIAGNOSIS
There are no tests to diagnose rosacea but your Doctor will examine your skin and ask you questions to determine whether or not you have rosacea. They might also test you to rule out lupus or allergies which both have similar symptoms. As I mentioned, many of our clients who have red, sensitive skin or a type of acne called inflamed acne come to us mistakenly thinking they have rosacea or acne rosacea because they have been wrongly diagnosed by a doctor or they have self diagnosed. This isn’t a surprise since Doctors and Dermatologists tend to spend very little time actually touching and getting to know our skin, lifestyle, habits, and skincare routines. Most of the time, we find that they don’t actually have rosacea and their skin is just raw and red from not having a proper skincare routine or they have one of the four types of inflamed acne which are also characterized by redness, swelling, and soreness.
TREATMENT
Just like acne, there is no cure for rosacea and it’s a condition that needs to be managed long term using a multi-targeted approach. Also, just like with acne, Dermatologists can be less than helpful and will likely spend 2 minutes barely looking at your skin before writing you one prescription after another. In my experience, Dermatologists and Doctors rarely take the time to really understand our particular manifestation of a condition and to put the time into developing a comprehensive treatment plan that is customized based on our unique skin type, rosacea type, and lifestyle factors. They will likely prescribe you a bunch of different topical and/or oral medications and they will just keep on prescribing until you land on one where the improvements you see outweigh the potential side effects. Some common treatments might include:
Antibiotics like doxycycline, tetracycline, or minocycline may reduce swelling, inflammation, and the acne like bumps that occur with Papulopustular Rosacea.
Isotretinoin is a very strong drug that may be prescribed under one of it’s brand names like Accutane, Absorica, Myorisan, Sotret, Zenatane, Amnesteem, or Claravis. Potential side effects include vision and hearing problems, birth defects, liver or pancreas problems, increased pressure inside the skull, and joint pain.
Topical treatments like Brimonidine
THE AES SOLUTION
Many of our clients with acne rosacea (subtype 2: Papulopustular Rosacea) have seen significant improvements with our prescription-free program using a combination of personalized product plans made up of balancing and nourishing skincare products and lifestyle coaching. Since most people who come to our clinic thinking they have rosacea actually just have irritated skin, inflamed acne,or PIH, we take a 3-step approach to determining whether or not they actually have rosacea:
The first step whether we are working with a client who has rosacea or acne is to rehabilitate any sensitivity and dryness using our skincare products made up of balancing, nourishing ingredients. This helps rule out sensitivity and irritation. If a client is local and able to come to our clinic, we will customize a product plan for them during the Initial Consultation but we also teach our long distance clients how to customize their own product plan based on where there skin is at on any given day through our Virtual Program and our e-course The 8 Steps To Clear Skin.
Once someone is on an appropriate product plan, the second step is to clear their acne with our prescription-free program which helps rule out regular acne vs. rosacea acne.
Once the acne is cleared, we target the PIH using specialized chemical peels and products which rules out the possibility that the “rosacea” is actually pigmentation.
If there is still remaining redness or other rosacea symptoms after all of these steps, then it can be deduced that rosacea is actually present. If you are curious to learn more, you can get in touch with any questions through our website or Instagram @aes_acneclinic.